We also examined the risk of intensive utilization in both including and excluding the 4 states that did not collect information on either prenatal visits or education in and found no differences in the characteristics associated with intensive use data available on request from the authors. Moreover, although the definition of a prenatal visit has remained constant, it is possible that the increase in diagnostic procedures may have led to some of these visits being counted inappropriately as prenatal visits, and thus inaccurately inflating the number of visits for some women.
The newer measures of prenatal care utilization indicate that there has been an increase in the number of visits that women receive that exceed recommendations by ACOG. While there has been success in increasing prenatal care utilization to high-risk women, the benefits of increasing obstetric care to low-risk women are less immediately apparent. Given that the rates of low birth weight and preterm birth in the United States have not improved over this same period, investigations of cost benefit should explore the varied short- and long-term outcomes that may be influenced by prenatal care use to more completely evaluate the impact of these trends.
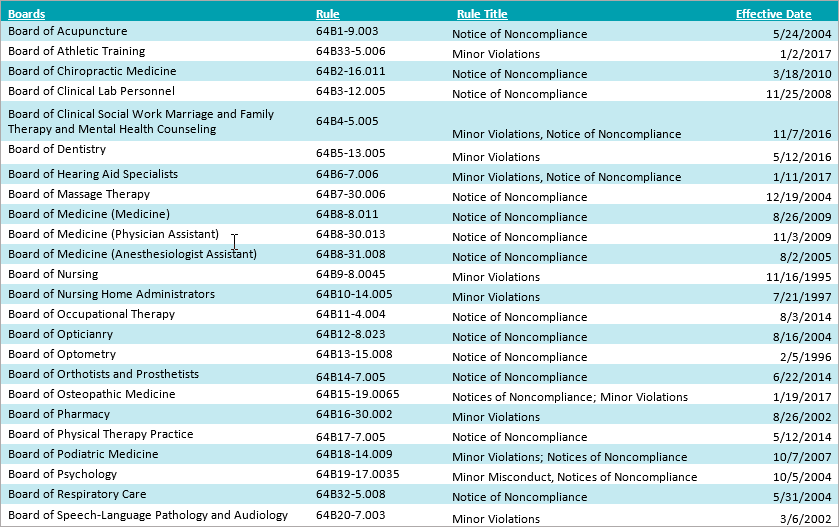
All Rights Reserved. View Large Download. The trends in adequate or intensive prenatal care utilization among low-risk women by prenatal care measure, to Table 1. Table 2.
Table 3. Table 4. Table 5. Ambulatory care visits to physician's offices, hospital outpatient departments, and emergency departments. Vital Health Stat Google Scholar. The effects of prenatal care upon the health of the newborn.
Duval County P.H.U.D.C.
Am J Public Health. Prenatal care and pregnancy outcome in an HMO and general population: a multivariate cohort analysis. Factors associated with birth weight: an exploration of the roles of prenatal care and length of gestation. Birth weight among women of different ethnic groups.
Family History and Genealogy Services
The differential effect of prenatal care on the incidence of low birth weight among blacks and whites in a prepaid health care plan. N Engl J Med. Weighing costs and benefits of adequate prenatal care for births in Missouri's Medicaid program, Public Health Rep. The relationship of prenatal care and pregnancy complications to birth weight in Winnipeg, Canada. Relation of the content of prenatal care to the risk of low birth weight: maternal reports of health behavior advice and initial prenatal care procedures.
Prenatal care utilization: its measurement and relationship to pregnancy outcome.
- franklin county ohio criminal information system.
- background information on the city of amsterdam.
- free consumer reports vehicles info.
- united states probation offender information form.
- A Genealogical History!
Am J Prev Med. Prenatal care utilization in Minnesota: patterns of concern and areas for improvement. Minn Med. The role of prenatal care in preventing low birth weight. Future Child. Does prenatal care improve birth outcomes? Obstet Gynecol. Institute of Medicine. Preventing Low Birth Weight. Access to Health Care in America. The role of obstetrical medical technology in preventing low birth weight. Effects of Medicaid eligibility expansion on prenatal care and pregnancy outcome in Tennessee.
Medicaid and prenatal care: necessary but not sufficient. US General Accounting Office. Infant death: an analysis by maternal risk and health care. In: Contrasts in Health Status. Vol 1. Report of final natality statistics, Mon Vital Stat Rep.
- Florida Public Records?
- Florida Adoption Reunion Registry | Florida Adoption Records.
- search engine to identify antique print.
- birth certificate from wayne county michigan.
- Certified Copies for Marriage License - Clerk of Courts - Miami-Dade County.
Trends in the Well-being of America's Children and Youth, Prenatal care in the United States, Quantifying the adequacy of prenatal care: a comparison of indices. American College of Obstetricians and Gynecologists. Standards for Obstetric-Gynecologic Services.
A comparison of two indices of adequacy of prenatal care utilization. A comparison of measures of prenatal care use. Med Care. National Center for Health Statistics. A method of imputing length of gestation on birth certificates. Vital Health Stat 2. Determinants of prenatal care use in Hawaii: implications for health promotion. Ultrasound during pregnancy: a discussion. Use of antenatal services in a controlled ultrasound screening trial. Acta Obstet Gynecol Scand.
Page not found - STEFMONT s.r.o
Change in obstetric practice in response to fear of litigation in the British Isles. Practice patterns of obstetricians and gynecologists in Jacksonville, Florida. J Fla Med Assoc. Practice changes in response to the malpractice litigation climate. Defensive medicine and obstetrics.
Increasing trends in plural births in the United States. Assisted reproductive technologies: estimates of their contribution to multiple births and newborn hospital days in the United States. Fertil Steril.
Search the Catalog
For every dollar spent—the cost-savings argument for prenatal care. The cost effectiveness of prenatal care in reducing low birth weight in New Hampshire. Health Serv Res. A cost-effectiveness analysis of strategies to reduce infant mortality. The quality of vital perinatal statistics data, with special reference to prenatal care. Paediatr Perinat Epidemiol. Sources of bias in prenatal care utilization indices: implications for evaluating the Medicaid expansion. Discordance between LMP-based and clinically estimated gestational age: implications for research, programs and policy. The validity of gestational age estimation by menstrual dating in term, preterm, and postterm gestations.
The status of birth certificate data in Georgia.